Dr. Parsons’ Personal Journey December, 2016
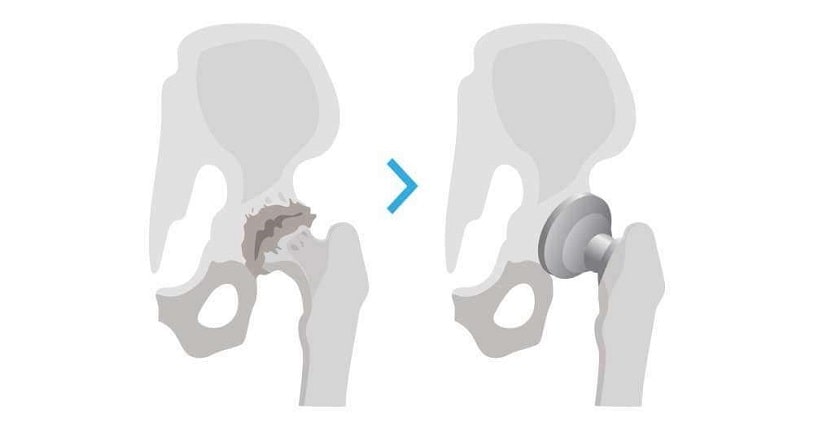
This past December 19th, I underwent bilateral total hip replacements. The week before going out for surgery and recovery, I performed surgery on 4 consecutive days in order to meet the demands of patients who were trying to get their surgery done before the end of the calendar year. About 10 of these cases were total hip replacements. Needless to say, it was a bit nerve racking to perform these operations and realize that in a few short days, I would undergo the same operation. Now 11 days post-surgery, I have had some time to reflect back over some observations as a patient that may prove useful given my “new” view from the other side of the operating table.
- Physical preparation is important. For me this included the following
- regular exercise roughtly 4 days a week to include both cardio and strength training. Exercises to improve core and hip stability will help one posteropatively. Working with a therapist before surgery will allow you to get training in the proper exercises and techniques.
- proper nutrition: this includes protein supplementation, Vitamin D (2000 IU daily) and Vitamin C s(2000mg daily) starting 6 weeks before surgery. This helps strengthen your bones but also provides building blocks for healing. These should be continued postoperatively for at least 3 months.
- other supplements that may be helpful for building a stronger immune system and blood count include zinc 50 mg daily and Vitamin B12 1000 mcg daily.
- for protein I prefer whey protein powder, which is readily available at most supermarkets and pharmacies. This can be used to create smoothies with fruit.
- probiotics are also important for immune health. I prefer Greek yogurt with real yogurt cultures. My preferred brand is Fage, also available in most supermarkets in the dairy section. Kefir is another good source. Both can be mixed with whey protein in a smoothie.
- reduction or cessation of alcohol intake. I stopped all intake 6 months before surgery. This helps to cleanse and detoxify the liver, which metabolizes pain medications and other medications after surgery. If your liver has a tolerance to these things, they will not work as well for you when you need them postoperatively. It is a good idea to continue abstinence for several months after surgery during the healing process as well.
- there are other modifiable risk factors that are well established and correlated with a higher risk of infection and other complications. Elective total joint surgery should ideally be delayed until patients have addressed these problems:
- poorly controlled diabetes. Ideally, the Hemoglobin A1C should be near 7.0 or less at the time of surgery.
- smoking should be stopped 3-4 weeks prior to surgery as it is strongly correlated with worse outcomes, including wound healing problems and infections.
- obesity: this is an epidemic! Ideally, one should delay surgery until the body mass index is 35 or less. Obesity correlates with many problems, including infection, wound healing problems, blood clots, premature implant failure, continued joint pain and others. If diet and exercise have not been successful, consider surgical weight loss options. Studies with large groups of patients have shown that those who undergo surgical weight loss prior to joint replacement have superior outcomes long term.
- Mental Preparation
- do your homework prior to surgery and know what your options are. This was a little easier for me because I do this for a living.
- Surgeon: hip replacement is a common operation in orthopedics, but you want to choose a surgeon who has performed hundreds of these operations and specializes in the joint replacements. Surgeons with this kind of experience can not only do the operation faster, they have a lower complication rate and they tend to employ rapid recovery protocols that expedite getting up and moving quickly.
- Hospital: choose a hospital that does at least 150 hip replacements or more yearly. Research shows that such hospitals have few complications and readmissions after surgery. It is also possible to find information online about hospital infection rates. Bear in mind that these numbers reflect all surgeons who do these operations at that hospital and not necessarily one individual surgeon.
- Approach: there are different ways to put in a hip replacement. They all work but may have different recovery rates. Know which one your surgeon uses and how many they have done. You do not want to be on the learning curve of a new technique.
- Implant: again, there are numerous implants on the market, including different bearing surfaces. Know what you are getting and what the track record of the implant is. Newer is not always better, and there are numerous examples in orthopedics where newer designs have been recalled because of premature failures.
- get your home and supplies ready in advance of the surgical date so you are not scrambling last minute.
- do your homework prior to surgery and know what your options are. This was a little easier for me because I do this for a living.
- Discharge planning: do this in advance. Know where you plan to go after surgery and have a goal in mind for when this is going to be.
- if you live alone and do not have many family or friends that can help you, it may make sense to spend some time in an inpatient rehabilitation facility. There are often several different local options. Visit these in advance and talk to other patients and your surgeon about their experience or any specific preferences.
- if you plan on going straight home, get your home ready and supplies ready in advance.
- deal with loose rugs and power cords that may pose a fall risk.
- make sure you have a shower that can accommodate you safely (shower chair or rails) and that you can get in and out of safely.
- install your raised toilet seat in advance and make sure it is stable and safe.
- stock up on basic supplies including plenty of fluid like Gatorade or Powerade to help keep you well hydrated when you get home.
- make sure you have your walker and your cane adjusted and at the ready as well as your other necessities like a grabber, sock tool, long shoe-horn etc. These can be purchased as a kit from places like Amazon.com or other medical supply companies.
- get your prescriptions in advance so you have your medications already at home. Understand what your surgeon’s expectations are regarding pain management and whether you have any specific concerns regarding medication intolerance etc…
- Expectation Management:
- there is no surgery that can make you 100% of normal and there will always be patients you meet that tell you they were back to playing 18 holes of golf after 2 weeks. Do not go into the surgery thinking you are going to be one of these exceptional patients. In all likelihood, their situation was different than yours.
- it is important to realize that surgery and recovery are together a process that can take many month for complete recovery and during this time you must remain engaged and motivated to keep yourself optimized and to participate actively in the recovery process including daily exercise.
- even as a physician, I have had numerous patients tell me prior to my own surgery the importance of listening to your doctor and your therapist and the importance of doing your rehabilitation homework. You will not get better automatically.
- you will have setbacks along the way – expect it and do not get upset about it. Progress will be measured in weeks, not days or hours.
- you are going to be awakening muscles that have not been properly used in some time, and you are going to have to break bad habits that you have developed because your arthritic joint has caused you to compensate in some manner that you may not be consciously aware of. Breaking these bad habits takes time and effort.
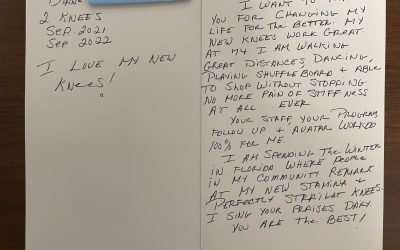
- set long term goals for what you want to get back to, realizing that there may be some activity restrictions after joint replacement. In my case, it is skiing, recognizing that I may never be able to attack the slopes with the same degree of difficulty as I once did. Realizing that I still like to get outside in the mountains in the winter is enough of a silver lining to give me a long-term target to shoot for.
- realize that you will likely not be able to return to the same activities that may have landed you in the operating room in the first place. In my case, marathon running, ultramarathon running, trail marathoning, aggressive skiing, ski mountaineering and long hours on my feet in the operating room (along with some genetic predisposition) contributed to the demise of my hips. I will not be able to marathon run ever again, but I will be able to mountain bike, hike, cross-country ski, ski in more moderation and still do a host of other activities that can provide great enjoyment. Focus on the positives and accept that you will have to make some activities compromises if you want your new hips to last a long time.
- Infection Prevention: infection present(s) a devastating complication after joint replacement and may require prolonged IV antibiotics and possibly implant removal. Taking measures in advance can help lower the risk.
- Chlorhexidine wipes can be used starting several days before surgery to lower the count of bacteria on the skin. Some joint replacement programs will provide these to the patient while others do not. If not, consult your pharmacist about how to obtain them, and start by wiping down your whole body twice daily starting 3 days before surgery.
- Mupirocin nasal ointment: this is an ointment that can be used to swab one’s nostrils starting 5 days before surgery. It reduces Staph bacterial contamination. Some joint programs will do a nasal swab and check patients for Staph colonization in the nose beforehand. Others may not do this. A prescription is required for this ointment. If your surgeon or program does not perform a nasal swab, ask them about this option.
- see above about modifiable risk factors
- do not shave the morning of surgery
- Morning of Surgery
- clear liquids are allowed up to 2 hours prior to surgery, and research has shown that it is actually beneficial in terms of preventing dehydration for patients who may have surgery later in the day. Clear liquids means no heavy juices, no dairy, no cola. Water is preferred.
- bring a book, game, movie or other material to keep your mind distracted. Depending on the program, they may call you in several hours before the actual surgery and there is often a lengthy waiting period. Realize that surgery is not an exact science in terms of scheduling and there may be delays. The less you are aggravated by this, the better.
- avoid catastrophic thinking. You have made it this far, and if you have done the measures above, you should have faith and trust in your surgeon. The vast majority of cases are uneventful and without complication. Realize that statistics are widely in your favor, particularly if you have taken steps to optimize and prepare yourself.
- Postoperative Course in Hospital
- I think everyone’s experience with this is different so I will just add some highlights
- Distraction: the best way to avoid the sensation of pain is to flood your mind with other stimuli. Most people do not sleep well in the hospital because the beds are uncomfortable and the nurses have to check your vital signs every hour. Bring something to fill the time like Audiobooks, movies, puzzles, games etc…The more you focus on these things, the less your mind will focus on the pain.
- Hydration: even though you get a lot of fluid by IV, the body still gets relatively dehydrated around the time of surgery. Drink a lot of fluid but not too much. Brining some Gatorade into the hospital with you is not a bad idea. I drank too much free water which later causes quite a bit of swelling as it leaked out into my tissues. Overhydration can cause swelling and even heart failure in healthy people.
- Sit before you stand. Patients are prone to low blood pressure after surgery and sudden changes in position can cause a rapid drop in the blood pressure. Change positions slowly and make sure your head is clear before doing anything that requires effort. Always call for help.
- Eat food. You need energy to rehabilitate and heal. You may not have much of an appetite after surgery but getting some nutrition and energy in your body is key getting better. If you do not like hospital food, consider having someone bring in something from the outside.
- The nurses and LNAs are there to help you. Some people feel embarrassed calling for help like it is a sign of weakness. These people make a living caring for people who need help. Do not hesitate to call them if needed. On the other hand, realize that certain requests take time. New medications have to be ordered through the physician and then sent to the pharmacy and back to the floor. It make take 45 minutes before you get it. This is not bad nursing care. This is the normal course of how information flows in the hospital.
- Set a goal of getting out and try hard to stick to it. Pain is not a reason to stay in the hospital. Many times you can manage your pain more effectively in the comforts of your own home. You can also sleep better in the comforts of your own bed. Hospitals are full of sick people and bad bacteria, there earlier you get out the better. I left the day after I had both of my hips done because the hospital bed was so uncomfortable I could not stand another night in it. I did far better at home with my dog to comfort me.
- The First Few Weeks
- continue good nutrition, adequate hydration and abstinence from alcohol, smoking or any other substances that may impair your mind of healing process.
- try to get back to a fairly regular routine of bathing, dressing etc…the sooner you feel some semblance of normalcy, the less you will feel like a “patient” and more like a “person”
- try to wean off of strong pain medications sooner rather than later. These medications cause sedation and constipation. Supplement them with Tylenol and anti-inflammatory medications.
- keep yourself on a good bowel regimen including high fiber foods, stool softeners, prune juice etc…constipation can be worse than pain and getting back to regular bowel habits is important for general healing
- exercise regularly but keep in mind that your body is recovering
- you will be more tired than usual. Listen to your body’s need for rest
- you will have good and bad days. Do not dwell on setbacks.
- do not overtax your mind.
- It is normal to feel excessively fatigued after surgery particular in terms of mental focus. Things like reading may be difficult for a few days to weeks.
- This is normal and do not force your mind to tackle task which it does not feel ready to pursue.
- Long-Term
- Maintenance Exercise: Rehabilitation is not done when you are discharged from physical therapy. Multiple studies demonstrate that improvement continues up to and past one year if you continue a maintenance regimen of exercises. As with many things in life, strength goes quickly and comes back slowly and bad habits are hard to break. Be persistent
- Activity Modification: joint replacement prostheses do not last forever. You should look at this operation as a long term investment. If well taken care of, a modern hip replacement will likely last beyond 20 years. If however, you subject your prosthesis to the same physical demands that may have necessitate a premature joint replacement to begin with, you can wear it out much fast and will require revision surgery. The same fact goes for obesity. Failure to correct ones weight will lead to premature wear of the implant. You do not have to treat your implant like fine chine but on the other hand, try not to abuse your hips.